On October 2, 2016, my son Myles, then 4 months old, had a fever. His older sister had just been sick, so my husband and I thought Myles had caught a bug from her. Poor little guy. I guess that’s how it goes when you have multiple kids with exposure to a lot of germs in one house.
About a month later, Myles had a heart attack. That’s right: a heart attack.
What in the world happened over the course of those 36 days? Kawasaki Disease. A blotchy rash, a high, prolonged fever, bloodshot eyes, joint pain, and cracked/bloody lips. Kids get strange rashes, right? And unexplained fevers. But what about when all of the above show up together? Then you’re looking at the key symptoms of Kawasaki Disease (KD).
The Kawasaki Disease Foundation describes KD this way:
Kawasaki disease (KD), also known as Kawasaki syndrome, is a serious illness characterized by inflammation of blood vessels throughout the body that primarily affects young children and infants. Kawasaki disease is the leading cause of acquired heart disease in children. Although about 80 percent of patients are under five years of age, older children and teenagers can also get KD, but this is uncommon. KD is more common in boys than girls and the majority of cases are diagnosed in the winter and early spring. It is not contagious.
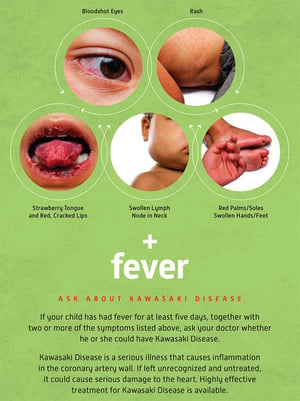 If treated early, KD is less likely to have lasting effects on a child’s life. That’s where providers come in. Know the signs.
If treated early, KD is less likely to have lasting effects on a child’s life. That’s where providers come in. Know the signs.
Our daily life now includes five medications: three that help Myles’ heart to function well and keep his blood pressure low, and two blood thinners to prevent another clot (which caused his heart attack). One of the blood thinners he’s on requires a twice-daily injection into his thigh. It causes bruising at the site, so both of his thighs are constantly filled with bruises of varying sizes.
Myles is now two years old. We all know how adventurous two year olds can be! Because he’s on blood thinners, Myles will have limitations as he gets older because of the risk of bruising and bleeding. It’s scary and something we take one day at a time.
Child care providers play such a key role in the life of a child. But if you’re reading this, you already know that! While KD is rare, more than 5,000 children in the United States are diagnosed with it each year and that number is rising. One of them could be a child you care for and you can make a difference. The most important part about treating KD is catching and treating it early. The ideal time to begin treatment is within 10 days after a fever begins.
After that, the chance of severe and long-term complications increases significantly.
There is no diagnostic test for KD. It is diagnosed by piecing together the symptoms and checking the heart via echocardiogram (ultrasound) for inflammation of the blood vessels and arteries.
So how can providers help? If you are aware that a child in your program 1) has been out with a fever for five or more days and 2) also has any combination of the symptoms listed above, talk to the family. Ask if the child’s physician has ruled out KD.
If you would like an awareness poster to hang at your center, share with families or colleagues, or even hang in your office, visit the KD Foundation online.